In the diagnosis and treatment of biliary diseases, the development of endoscopic technology has consistently focused on the goals of greater precision, less invasiveness, and greater safety. Endoscopic retrograde cholangiopancreatography (ERCP), the workhorse of biliary disease diagnosis and treatment, has long been widely accepted for its non-surgical and minimally invasive nature. However, when faced with complex biliary lesions, a single technique often falls short. This is where percutaneous transhepatic cholangioscopy (PTCS) becomes a crucial complement to ERCP. This combined “dual-scope” approach transcends the limitations of traditional treatments and offers patients a completely new diagnostic and treatment option.
ERCP and PTCS each have their own unique skills.
To understand the power of dual-scope combined use, one must first clearly understand the unique capabilities of these two instruments. Although both are tools for biliary diagnosis and treatment, they employ distinct methods, creating a perfect complement.
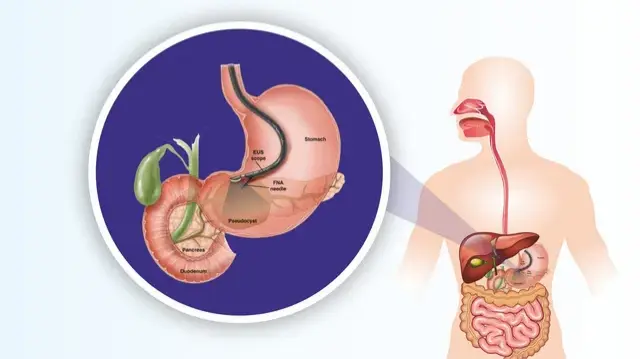
ERCP: An Endoscopic Expertise Entering the Digestive Tract
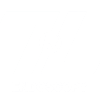
ERCP stands for Endoscopic Retrograde Cholangiopancreatography. Its operation is akin to a roundabout way of doing things. The doctor inserts a duodenoscope through the mouth, esophagus, and stomach, ultimately reaching the descending duodenum. The doctor locates the intestinal openings of the bile and pancreatic ducts (the duodenal papilla). A catheter is then inserted through the endoscopic biopsy port. After injecting a contrast agent, an X-ray or ultrasound examination is performed, enabling a visual diagnosis of the bile and pancreatic ducts.
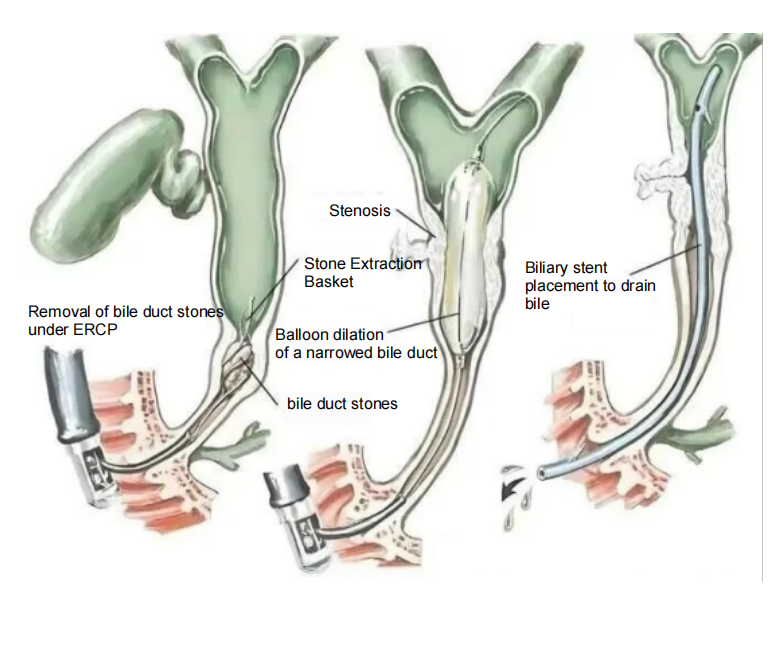
On this basis, ERCP can also perform a range of therapeutic procedures: for example, dilating narrowed bile ducts with a balloon, opening blocked passages with stents, removing stones from the bile duct with a stone removal basket, and obtaining diseased tissue for pathological analysis using biopsy forceps. Its core advantage lies in the fact that it operates entirely through the natural cavity, eliminating the need for surface incisions. This allows for rapid postoperative recovery and minimal disruption to the patient’s body. It is particularly suitable for treating bile duct problems close to the intestine, such as stones in the middle and lower common bile duct, lower bile duct strictures, and lesions at the pancreatic and bile duct junction.
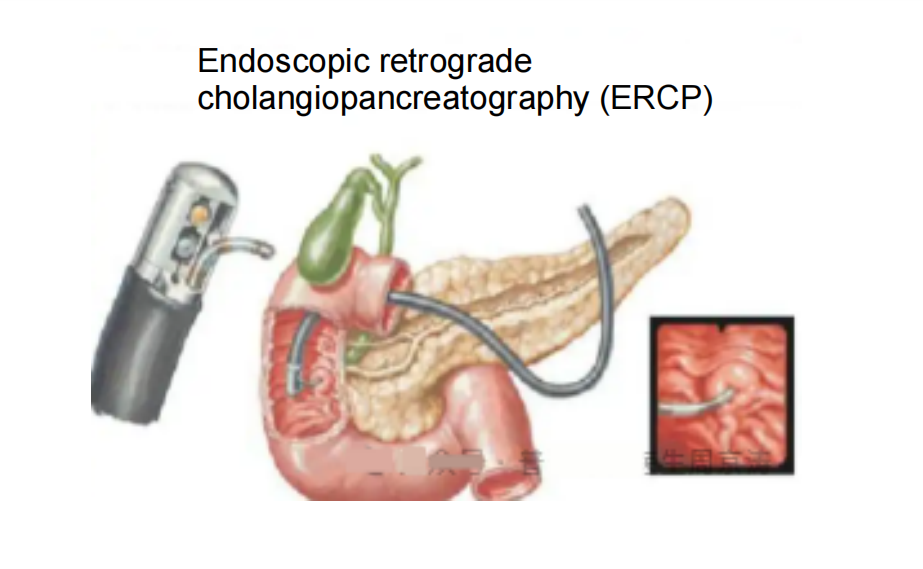
However, ERCP also has its “weaknesses”: if the bile duct obstruction is severe and bile cannot be discharged smoothly, the contrast agent will have difficulty filling the entire bile duct, which will affect the accuracy of the diagnosis; for intrahepatic bile duct stones (especially stones located deep in the liver) and high-positioned bile duct stenosis (close to the liver hilum and above), the treatment effect is often greatly reduced because the endoscope “cannot reach” or the operating space is limited.
PTCS: A Percutaneous Pioneer Breaking Through the Liver’s Surface
PTCS, or percutaneous transhepatic choledochoscopy, employs an “outside-in” approach, in contrast to the “inside-out” approach of ERCP. Under ultrasound or CT guidance, the surgeon punctures the skin on the patient’s right chest or abdomen, precisely traversing the liver tissue and accessing the dilated intrahepatic bile duct, creating an artificial “skin-liver-bile duct” tunnel. A choledochoscope is then inserted through this tunnel to directly observe the intrahepatic bile duct while simultaneously performing treatments such as stone removal, lithotripsy, dilation of strictures, and stent placement.
PTCS’s “killer weapon” lies in its ability to directly reach intrahepatic bile duct lesions. It is particularly adept at addressing “deep problems” difficult to reach with ERCP: for example, giant bile duct stones exceeding 2 cm in diameter, “multiple stones” scattered across multiple intrahepatic bile duct branches, high-positioned bile duct strictures caused by tumors or inflammation, and complex complications such as anastomotic stenosis and bile fistulas that occur after biliary surgery. Furthermore, when patients are unable to undergo ERCP due to reasons such as duodenal papillary malformation and intestinal obstruction, PTCS can serve as an alternative, rapidly draining bile and alleviating jaundice, thereby buying time for subsequent treatment.
However, PTCS is not perfect: since it requires puncture on the body surface, complications such as bleeding, bile leakage, and infection may occur. The postoperative recovery time is slightly longer than ERCP, and the doctor’s puncture technology and image guidance accuracy are extremely high.
A Powerful Combination: The Logic of “Synergistic Operation” with Dual-Scope Combination
When the “endovascular advantages” of ERCP meets the “percutaneous advantages” of PTCS, the two are no longer limited to a single approach, but instead form a diagnostic and treatment framework that “strikes both inside and outside the body.” This combination is not a simple addition of technologies, but rather a personalized “1+1>2″ plan tailored to the patient’s condition. It primarily consists of two models: “sequential combined” and “simultaneous combined.”
Sequential Combination: “Open the Pathway First, Then Precise Treatment”
This is the most common combination approach, typically following the principle of “drainage First, Treatment Later.” For example, for patients with severe obstructive jaundice caused by intrahepatic bile duct stones, the first step is to establish a biliary drainage channel through PTCS puncture to drain the accumulated bile, relieve liver pressure, reduce the risk of infection, and gradually restore the patient’s liver function and physical condition. Once the patient’s condition stabilizes, ERCP is then performed from the intestinal side to remove stones in the lower common bile duct, treat lesions in the duodenal papilla, and further dilate the bile duct stricture using a balloon or stent.
Conversely, if a patient undergoes ERCP and is found to have residual liver stones or high-level stenosis that cannot be treated, PTCS can be used to complete the “finishing work” later. This model offers the advantage of a “step-by-step approach with manageable risks,” making it particularly suitable for patients with complex conditions and pre-existing health conditions
Simultaneous Combined Operation: “Simultaneous Dual-scope Operation,
Single-Stop Solution”
For patients with a clear diagnosis and good physical tolerance, doctors may opt for a “simultaneous combined” procedure. During the same surgery, the ERCP and PTCS teams work together. The ERCP surgeon uses the endoscope from the intestinal side, dilating the duodenal papilla and placing a guidewire. The PTCS surgeon, guided by imaging, punctures the liver and uses the choledochoscope to locate the ERCP-placed guidewire, achieving precise alignment of the “inner and outer channels.” The two teams then collaborate to perform lithotripsy, stone removal, and stent placement.
The greatest advantage of this model is that it addresses multiple issues with a single procedure, eliminating the need for multiple anesthesia and surgeries, significantly shortening the treatment cycle. For example, for patients with both intrahepatic bile duct stones and common bile duct stones, PTCS can be used simultaneously to clear the intrahepatic stones and ERCP to address the common bile duct stones, eliminating the need for patients to undergo multiple rounds of anesthesia and surgery, significantly improving treatment efficiency.
Applicable Scenario: Which Patients Require Dual-Scope Combination?
Not all biliary diseases require dual-scope combined imaging. Dual-scope combined imaging is primarily suitable for complex cases that cannot be addressed with a single technique, primarily including the following:
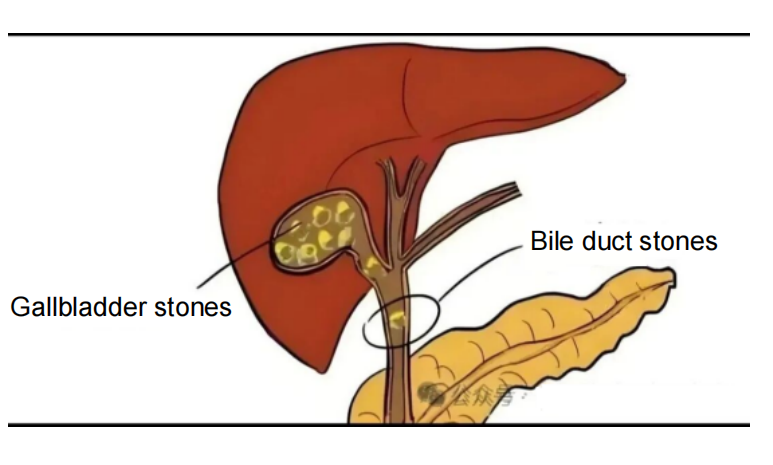
Complex bile duct stones: This is the primary application scenario for dual-scope combined CT. For example, patients with both intrahepatic bile duct stones (especially those located in remote locations such as the left lateral lobe or right posterior lobe of the liver) and common bile duct stones; patients with hard stones exceeding 2 cm in diameter that cannot be removed by ERCP alone; and patients with stones lodged in narrowed bile ducts, preventing the passage of ERCP instruments. Using dual-scope combined CTCS, CTCS “breaks up” large stones and clears branching stones from within the liver, while ERCP “clears” the lower passages from the intestine to prevent residual stones, achieving “complete stone clearance.”
High-level bile duct strictures: When bile duct strictures are located above the hepatic hilum (where the left and right hepatic ducts meet), ERCP endoscopes are difficult to reach, making it difficult to accurately assess the severity and cause of the stricture. In these cases, PTCS allows direct visualization of the stricture through intrahepatic channels, allowing biopsies to confirm the nature of the lesion (such as inflammation or tumor) while simultaneously performing balloon dilatation or stent placement. ERCP, on the other hand, allows for the placement of a stent below, which acts as a relay for the PTCS stent, ensuring unobstructed drainage of the entire bile duct.
Postoperative complications of biliary surgery: Anastomotic stenosis, bile fistula, and residual stones may occur after biliary surgery. If the patient has severe intestinal adhesions after surgery and ERCP is not possible, PTCS can be used for drainage and treatment. If the anastomotic stenosis is located high and ERCP cannot fully dilate, PTCS can be combined with bilateral dilation to improve the success rate of treatment.
Patients who cannot tolerate a single surgery: For example, elderly patients or patients with severe cardiopulmonary diseases cannot withstand a long single surgery. The combination of double mirrors can split the complex operation into “minimally invasive + minimally invasive”, reducing surgical risks and physical burden.
Future Outlook: The “Upgrade Direction” of Dual-Scope Combination
With technological advancements, the combination of ERCP and PTCS continues to evolve. On the one hand, advances in imaging technology are enabling more precise punctures and procedures. For example, the combination of intraoperative endoscopic ultrasound (EUS) and PTCS can visualize the internal structure of the bile duct in real time, reducing puncture complications. On the other hand, innovations in instruments are making treatment more efficient. For example, flexible choledochoscopes, more durable lithotripsy probes, and bioresorbable stents are enabling dual-scope combination to address more complex lesions.
Furthermore, “robot-assisted dual-scope combined” has emerged as a new research direction: by using robotic systems to control endoscopes and puncture instruments, doctors can perform delicate procedures in a more comfortable environment, further improving surgical precision and safety. In the future, with the increasing adoption of multidisciplinary collaboration (MDT), ERCP and PTCS will be further integrated with laparoscopy and interventional therapies, providing more personalized and high-quality diagnosis and treatment options for patients with biliary diseases.
The dual-scope combination of ERCP and PTCS breaks the limitations of a single-pathway approach for biliary diagnosis and treatment, addressing numerous complex biliary diseases with a minimally invasive and precise approach. The collaboration of this “talented duo” not only reflects the advancement of medical technology but also embodies the patient-centered approach to diagnosis and treatment. It transforms what once required major laparotomy into minimally invasive treatments with less trauma and faster recovery, allowing more patients to overcome their diseases while maintaining a higher quality of life. We believe that with continued technological breakthroughs, the dual-scope combination will unlock even more capabilities, bringing new possibilities to the diagnosis and treatment of biliary diseases.
We, Jiangxi Zhuoruihua Medical Instrument Co.,Ltd., is a manufacturer in China specializing in the endoscopic consumables, include GI line such as biopsy forceps, hemoclip, polyp snare, sclerotherapy needle, spray catheter, cytology brushes, guidewire, stone retrieval basket, nasal biliary drainage catheter, and Sphincterotome etc. which are widely used in EMR, ESD, ERCP.
Our products are CE certified and with FDA 510K approval, and our plants are ISO certified. Our goods have been exported to Europe, North America, Middle East and part of Asia, and widely obtains the customer of the recognition and praise!
Post time: Nov-14-2025